Exploring the Utility of Drug-Induced Sleep Endoscopy in the Management of Obstructive Sleep Apnea
One of the main challenges of surgical treatment in Obstructive Sleep Apnea (OSA) is identifying the correct site of upper airway obstruction in an individual patient.
Drug-Induced Sleep Endoscopy (DISE) in sedated patients with obstructive sleep apnea is the technique of choice for revealing anatomic and dynamic collapsible areas.
What Are the Advantages of The DISE Procedure?
Drug-Induced Sleep Endoscopy (DISE) represents a valuable adjunctive tool in the management of Obstructive Sleep Apnea (OSA), providing a dynamic assessment of upper airway obstruction during sleep in real-time.
While Continuous Positive Airway Pressure (CPAP) therapy remains the primary treatment modality, not all patients tolerate or benefit from it.
How Is The DISE Procedure Performed?
The patient is sedated similar to that of natural sleep. The medication given for sedation is propofol. Sedation allows the surgeons to look inside the throat using a long, thin tube-like camera known as a flexible fiberoptic laryngoscope or an endoscope.
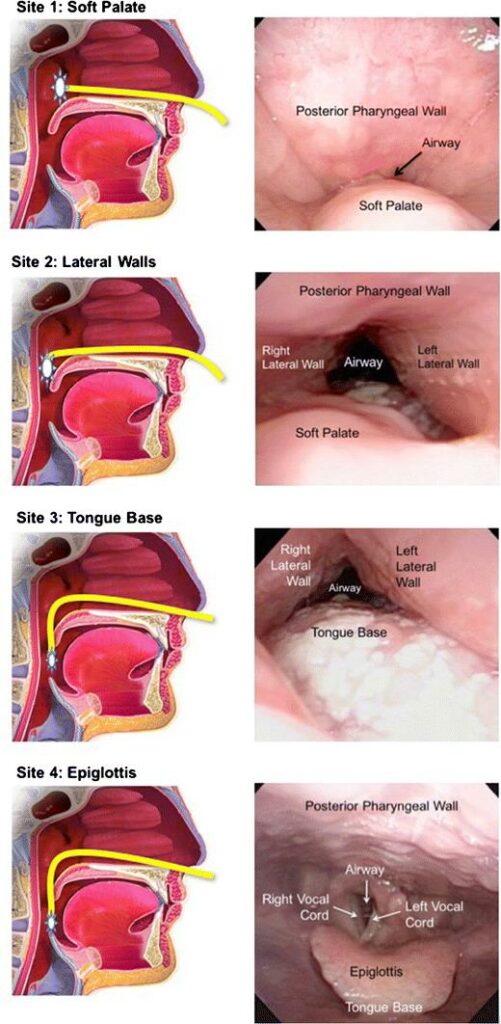
Once the anesthesiologist confirms that the patient is sedated and breathing, the surgeons place the laryngoscope through one of the nostrils and into the throat to examine the airway and nearby possible regions that can cause obstructive sleep apnea (OSA).
How Is It Different?
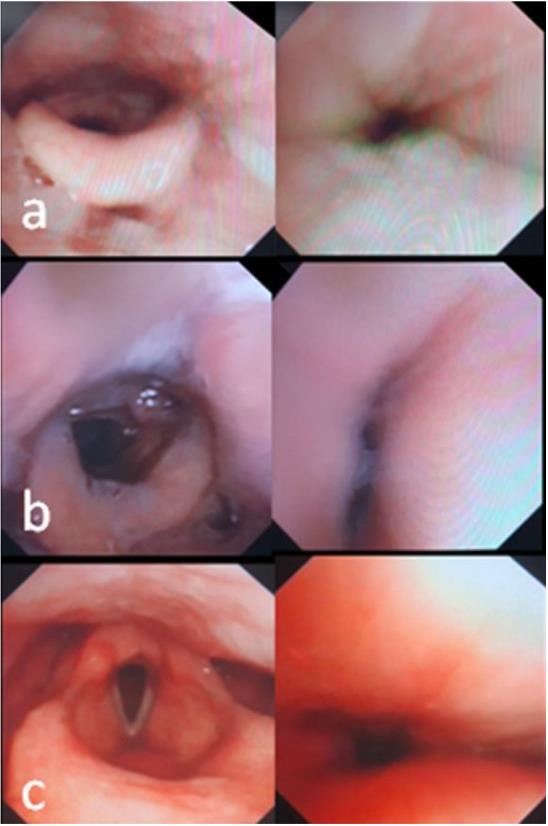
Unlike awake endoscopy, which assesses the static airway configuration, DISE provides real-time assessment of upper airway collapse patterns during sleep, mimicking physiological conditions encountered in OSA. The procedure is typically performed in an outpatient setting under the supervision of an experienced sleep physician and surgeon.
Mapping of dynamic upper airway collapse during sleep is a key point in OSA patients who are candidates for surgical treatment.

Clinical Utility of DISE in OSA Management
1. Identification of Anatomical Sites of Obstruction
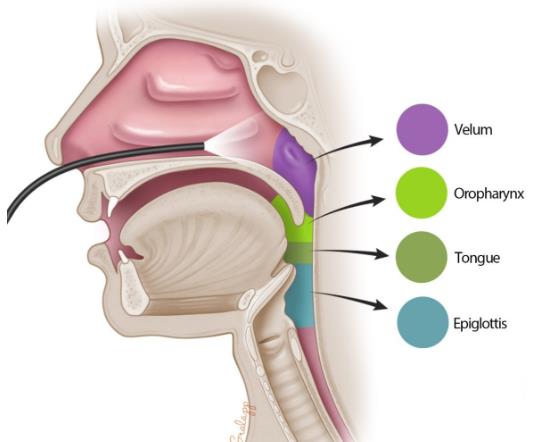
DISE enables precise localization of anatomical sites contributing to upper airway obstruction, including the soft palate, lateral pharyngeal walls, tongue base, and epiglottis. By visualizing the dynamic collapse patterns during sleep, DISE helps clinicians tailor surgical interventions, such as uvulopalatopharyngoplasty (UPPP), tongue base reduction, hypopharyngeal procedures, maxillomandibular advancement, etc. to target specific areas of obstruction.
2. Assessment of Multi-Level Obstruction
OSA often involves multi-level obstruction, where collapse occurs at multiple anatomical sites simultaneously or sequentially. DISE facilitates the identification of multi-level obstructions, guiding the selection of combination therapies or staged surgical procedures to address all contributing factors comprehensively.
3. Evaluation of Treatment Response
DISE can be valuable in assessing treatment response following surgical interventions or non-surgical therapies such as oral appliances or positional therapy. By comparing pre- and post-intervention endoscopic findings, clinicians can objectively evaluate the effectiveness of treatment and identify residual or recurrent obstructions requiring further intervention.
4. Patient Selection for Surgical Interventions
In patients considering surgical interventions for OSA, DISE aids in patient selection by identifying individuals most likely to benefit from specific procedures based on their pattern of airway collapse. Additionally, DISE helps mitigate the risk of selecting inappropriate candidates who may have non-anatomical contributors to OSA, such as central or mixed sleep apnea.